As Unmet Care Needs Grow, Streamlining Patient Access Becomes Critical
Redefining the care delivery pathway is becoming a focal point for providers as they juggle increasing consumer expectations with patient access and demand for value-based care, staffing shortages and burnout, and more provider competition.
But when redefining the care delivery pathway, providers must consider the other side of the healthcare journey: the patients struggling to navigate a complicated system to manage their own health—in a time when delayed care needs are building. According to a recent study, chronic disease burden will only continue to increase because “during the pandemic, many patients delayed or skipped necessary care, including physician visits and medical tests.”
Catching up with delayed care is compounding at a time when providers are doing their best to prioritize operational efficiencies with fewer resources. However, despite the increased demand for care, providers are also finding themselves in a paradox: long appointment lead times, yet provider capacity is underutilized. One client told us that roughly 10-30% of appointment slots are still going unused.
By simplifying access to care through intelligent scheduling technology, provider groups of all sizes and specialties are removing barriers to patient access and boosting provider utilization rates—and giving their patients the timely, quality care they need.
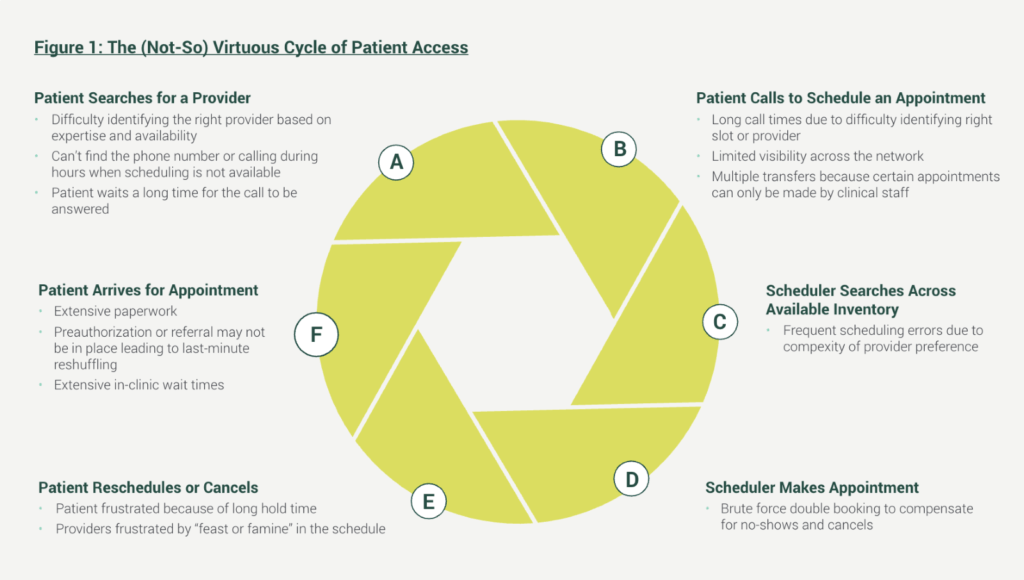
The (not-so) virtuous cycle of patient access
Switching the perspective of patient scheduling and access from the provider to the consumer illustrates how the traditional access cycle is prone to leakage, cancellations, and poorer patient experiences. The complexity of self-managing one’s health—determining providers in network with insurance, referrals needed, available time slots, further follow-up appointments—is not only overwhelming, but can lead to attrition and worsening health conditions due delays. In fact, nearly one in five healthcare consumers said that “managing their healthcare is more painful than doing taxes.”
In Figure 1, the current-state patient access cycle is detailed:
Navigating a healthcare system from behind closed doors is also what leads to a traffic jam of patients, increased no-shows, and unbalanced provider schedules. A 2019 stat poll by the Medical Group Management Association (MGMA) found that providers have looked to five strategies to solve the challenge of patient access:
- Extending clinic hours
- Modifying workflows
- Utilizing portal/online scheduling
- Hiring more providers and staff
- Upgrading technology
With staffing shortages predicted to increase for both clinical and administrative roles across all specialties, upgrading technology—such as the use of intelligent patient self-scheduling software—is rapidly becoming a low-risk, high-reward strategy.
“Our top priority with scheduling is to get patients in with the right doctor at the right location as quickly as possible,” said Kevin Deter, Chief Operating Officer at Peachtree Orthopedics. Read their story here.
Intelligent patient scheduling solutions free up staff time while filling provider time
The first step to streamlined patient access is removing unnecessary scheduling hurdles—such as a heavy reliance on staff time and knowledge—by implementing a tool that leverages rules-based scheduling automation to match provider preferences and available times, fill no-shows, create a wait list, and share this view across the organization at the click of a button.
This digital transition creates a more user-friendly experience that allows staff and patients to quickly and accurately find the right appointment, at the right time, with the right physician. In addition, a streamlined process reduces cumbersome manual workflows, errors, hold times, wait times, and unused slots.
Further, intelligent communication and engagement technology—such as patient appointment reminders, patient self-scheduling software, billing reminders, two-way messaging, and intake paperwork—can do more to help patients connect with the care they need, keep their appointments, and follow-up on payments and additional appointment scheduling.
Learn the full seven strategies for redefining patient access in Winning the Patient Access Game: 7 Ways Provider Groups Can Deliver More for Less with Centralized Scheduling.